“AIDS is a lot like ‘SNL’ ['Saturday Night Live'],” quipped comedian Pete Davidson last month, on the finale of the show’s 46th season. “It’s still here, it’s just no one’s gotten excited about it since the ’90s.”
Davidson’s joke came almost exactly 40 years after the first cases of a mysterious rash of infections among gay men in New York and Los Angeles — which would soon be recognized as AIDS — was first reported in the national news. It also pointed to an uncomfortable truth: Although AIDS is still a crisis, with an estimated 34,800 new HIV infections in the United States in 2019, Americans largely no longer treat it as such. The reason? Since the mid-1990s and the advent of highly effective drugs to treat HIV, the virus that causes AIDS, the epidemic has mostly come to affect those who have the least.
As 2021’s Pride Month comes to a close amid the continuing coronavirus pandemic, we should think about what it means to live through a pandemic that is fading from public view, even as it shapes and shortens the lives of vulnerable people.
In the early 1980s, the advent of a new, mysterious and deadly disease that was associated with gay men, drug users and Haitian immigrants amplified undercurrents of homophobia, racism, misogyny and xenophobia in American society. The mainstream media and all but a few policymakers were concerned about AIDS only insomuch as it posed a threat to the “general population,” meaning White, straight people. Some argued, quite seriously, that people with AIDS should be quarantined or tattooed, and evangelical Christian leaders such as Jerry Falwell described AIDS as “not just God’s punishment for homosexuals,” but “for the society that tolerates homosexuals.”
In the face of such hostility, people with AIDS and their allies cared for the sick and dying, filling in gaps in the social safety net that had been deliberately unraveled by President Ronald Reagan and his allies at all levels of government. At the time, there were no effective treatments available for the new disease. The FDA didn’t approve AZT, the first AIDS drug available in the United States, until six years into the epidemic, in 1987. It was not only highly toxic, but also expensive, costing $10,000 a year.
With so few treatments available, AIDS activists pressured government agencies to invest in research for new therapies, fought to speed up the approvals process for new drugs and pushed to make experimental medicines available to the sick. Calling for “drugs into bodies,” they advocated for biomedical solutions to the epidemic.
But many of those same activists also saw the disease as a political crisis, driven by corporate greed, societal neglect and indifference to the suffering of those most affected by the disease, including gay men, drug users and people of color. In 1987, the first demonstration by the AIDS Coalition to Unleash Power (ACT UP) targeted AZT manufacturer Burroughs Wellcome over the drug’s high price. A few months later, the group marched in New York City’s Gay Pride parade with a concentration-camp-themed float to make the point: AIDS was a genocide of neglect against groups that many Americans saw as undesirable or expendable.
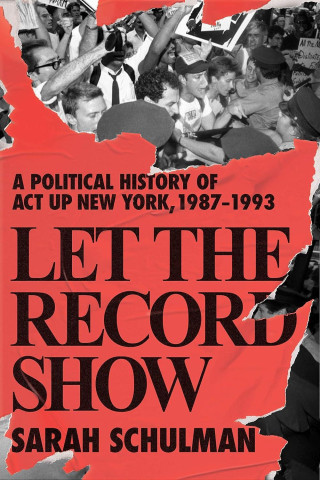
As Sarah Schulman details in her new book “Let the Record Show,” ACT UP members also fought to expand the case definition for the disease, which had initially prevented many women from being diagnosed and receiving the disability benefits available to people with AIDS. Some also pushed not just for new medications or an expanded definition of the disease, but for major policy changes, including a national health-care system. As Jim Eigo, a member of ACT UP recalled to Schulman in 2004, “A lot of us who were working in drug approval wanted to push the fight to universal health care and reforming things like Social Security, Medicare and Medicaid.”
The advent of protease inhibitors in the mid-1990s brought about a revolution in AIDS treatment. Whereas an HIV diagnosis was seen as a death sentence in the 1980s and early 1990s, today people with HIV who are receiving treatment have similar life expectancies as people who are HIV negative. Newer therapies also play an important role in the prevention of HIV transmission.
Yet a closer look at long-term trends shows that, while African Americans have been disproportionately affected by AIDS since the beginning of the epidemic, racial disparities became even more pronounced with the availability of protease inhibitors. In 1995, White Americans and African Americans made up roughly equal percentages of new AIDS diagnoses in the United States. Within a decade, new AIDS diagnoses among African Americans outpaced those among White Americans by almost 20 points.
That’s because highly effective HIV treatments are expensive, and most available to those who already have access to quality health care. For others, many of whom also suffer from what sociologist Celeste Watkins-Hayes calls “injuries of inequality” — discrimination in employment, unstable housing and racialized policing and incarceration — HIV treatment and prevention remains a significant challenge.
As activists have long argued, AIDS is a political crisis. Protease inhibitors changed the nature of the disease, but only for those with access to them — namely White, gay, middle class men. And while the Affordable Care Act did expand access to health care in the United States, especially for people with HIV, it fell far short of activists’ visions for universal health care. In the absence of larger policy change, we have come to treat AIDS as a biomedical problem, to be managed primarily through testing and treatment, while the underlying conditions that render some of us far more vulnerable than others persist.
The human cost of this approach to AIDS shows up in ongoing racial disparities in the epidemic. Forty-two percent of new HIV infections in 2019 were among African Americans, who make up just 13 percent of the total population, and 26 percent of those new infections were among Black men who have sex with men, including those who identify as gay or bisexual. The AIDS epidemic is also concentrated among poor communities, particularly those in the South. Not surprisingly then, as journalist Linda Villarosa has reported, poor Black gay and bisexual men in the South are among those at the greatest risk.
As AIDS has increasingly affected those with the least access to resources, education and health care, we have paid less and less attention to the disease. In short, AIDS settled into the cracks in our society, tracing the lines of inequality and injustice that limit the lives — and life expectancies — of too many of us.
If AIDS has, over time, settled into the cracks in our society, the coronavirus threw those cracks into sharp relief. A recent analysis of mortality data through November 2020 found that Black Americans were 3.6 times more likely, and Hispanic Americans 2.8 times more likely, to die of covid-19 than their White counterparts.
These same disparities are also shaping efforts to distribute the coronavirus vaccine. Vaccination rates for Black and Hispanic Americans lag behind those for White Americans, while efforts to vaccinate incarcerated people vary widely from state to state. Many of the states with the lowest vaccination rates are those in the Deep South, with weak social safety nets and large Black populations.
That’s no accident. The small-government ideology that directs their politics stems from the idea that poor Black communities are undeserving of help or sympathy.
When activists said that AIDS was a political crisis, they meant that the epidemic was driven by greed, neglect and indifference. The same can be said of the coronavirus, a pandemic made worse by the greed of corporations that drove people back to work in conditions that make them sick, the neglect that leaves poor and minority communities vulnerable to the virus and indifference to the death and suffering that the pandemic has wrought on those same communities. And it seems entirely likely that in the United States, covid-19, like AIDS, will settle further into communities such as these, while the rest of the country moves on.
As the country opens back up, we may think about how Americans will look back on the coronavirus outbreak in the years ahead. Will they see it as a turning point, after which Americans embraced major policy changes to ameliorate the inequalities that epidemic illnesses, like covid-19 and AIDS, have laid bare? Or will they see it as a missed opportunity, a hardship too soon forgotten, after which the country stumbled into the next public health crisis, no better off than before?